[fusion_builder_container hundred_percent=”no” equal_height_columns=”no” menu_anchor=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=”” background_color=”” background_image=”” background_position=”center center” background_repeat=”no-repeat” fade=”no” background_parallax=”none” parallax_speed=”0.3″ video_mp4=”” video_webm=”” video_ogv=”” video_url=”” video_aspect_ratio=”16:9″ video_loop=”yes” video_mute=”yes” overlay_color=”” video_preview_image=”” border_color=”” border_style=”solid” padding_top=”” padding_bottom=”” padding_left=”” padding_right=”” type=”legacy”][fusion_builder_row][fusion_builder_column type=”1_1″ layout=”1_1″ background_position=”left top” background_color=”” border_color=”” border_style=”solid” border_position=”all” spacing=”yes” background_image=”” background_repeat=”no-repeat” padding_top=”” padding_right=”” padding_bottom=”” padding_left=”” margin_top=”0px” margin_bottom=”0px” class=”” id=”” animation_type=”” animation_speed=”0.3″ animation_direction=”left” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” center_content=”no” last=”true” min_height=”” hover_type=”none” link=”” border_sizes_top=”” border_sizes_bottom=”” border_sizes_left=”” border_sizes_right=”” first=”true”][fusion_text columns=”” column_min_width=”” column_spacing=”” rule_style=”default” rule_size=”” rule_color=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” class=”” id=””]
Single Embryo Transfer commonly known as SET, is a complex medical procedure, in which a single embryo is selected and transferred to the uterus or fallopian tube for improved chances of conceiving. The selected embryo may be a fresh embryo or a cryopreserved embryo from a previous in vitro fertilization (IVF) cycle.
According to recent research studies that evaluated the success rates of women choosing to undergo assisted reproductive technology (ART), younger women who chose SET had a similar number of live birth deliveries per embryo. Those who chose to transfer multiple embryos, on the other hand, had a similar number of birth deliveries but most of the infants were delivered as singletons as opposed to the expected twins or multiples.
Women who elect to transfer multiple embryos increase threats to their own health because of the risk associated with carrying multiples. For instance, carrying twins or multiples increases the chances of preterm labor and birth, meaning the babies will be delivered before their bodies and organ systems have fully developed and matured. Babies who are born prematurely have a lower survival rate than those who were not born prematurely. Women with multiple pregnancies are more likely develop pregnancy complications such as high blood pressure, diabetes, and anemia. They are also more likely to need a Cesarean section, which requires long periods of recovery and may increase the risk of hemorrhage before and after deliver. Additionally, a miscarriage is more likely to occur when carrying multiple babies. For these reasons, most physicians and reproductive organizations recommend single embryo transfer.
Regarding the success of SET with women who had high chances of success with ART, the American Society for reproductive Medicine (ASRM) and the Society for Assisted Reproductive Technology (SART) developed guidelines for physicians to regard during their practice. The guidelines include allowing single embryo transfers to be considered for patients with favorable chances, which includes women who are 35 or younger and have eggs or embryos of high quality.
In the field of Assisted Reproduction, there are very few challenges left to face. However, one of these challenges, and arguably the most important is selecting embryos that has the best chance of implanting and creating a healthy baby. The current solution to this is to use morphological (microscopic) grading on day 2 or 3 after fertilization. Another option is using genetic testing like fluorescence in-situ hybridization (FISH) to help locate the positions of specific DNA sequences on chromosomes. Unfortunately, both methods lack sensitivity and specificity. These are the main reasons many IVF specialists choose to transfer multiple embryos at a time to increase chances of successful conceiving. But as mentioned earlier, multiple pregnancy increases the risks of complications in both the women and the babies.
[/fusion_text][fusion_text columns=”” column_min_width=”” column_spacing=”” rule_style=”default” rule_size=”” rule_color=”” content_alignment_medium=”” content_alignment_small=”” content_alignment=”” hide_on_mobile=”small-visibility,medium-visibility,large-visibility” sticky_display=”normal,sticky” class=”” id=”” margin_top=”” margin_right=”” margin_bottom=”” margin_left=”” font_size=”” fusion_font_family_text_font=”” fusion_font_variant_text_font=”” line_height=”” letter_spacing=”” text_color=”” animation_type=”” animation_direction=”left” animation_speed=”0.3″ animation_offset=””]To help improve the embryo selection process embryologists have developed certain protocols.
Embryo Grading
Most IVF clinics fertilize the women’s eggs and culture the embryos in groups. While the embryos are developing, the embryologists will monitor their health prior to choosing one for transfer. The embryos are graded depending on the growth rate, which help indicate the presence of chromosomal issues, as well as the appearance of cells and fragmentation, which suggest an inherent defect in the egg. Those with uneven cell division and higher degrees of fragmentation are graded lower and lead to lower likelihood of pregnancy.
Blastocyst Embryo Transfer
An embryo that develops successfully to day 5 or 6 of life is referred as blastocyst. After day 5, blastocyst evaluations take place where the embryos are graded depending on their development. Most embryos that fail to develop into a healthy blastocyst in lab itself are chromosomally abnormal. On day 5, the embryologist will investigate the fragmentation percentage, synchrony of cell division, and evenness of cell division among the embryos. The embryos that reach the blastocyst stage are less likely to have chromosomal abnormalities and deemed more viable. Studies have shown that blastocyst transfer have a higher rate of implantation and successful pregnancy than transfers involving day 2 or 3 embryos. Thus, the best embryo at the blastocyst stage will be chosen for the embryo transfer, while the others will be frozen if a second try is necessary.
Along with today’s current practice, three recent developments in the IVF field improve the chances of success among good candidates. The first two are regarded as standard for implementation. The third offers greater enhancement for success but has yet to be regarded as a standard requirement.
- Extended Embryo Culturing Methods: The latest extended and advance developed embryo culture techniques over the span of last 10 years make it possible to successfully grow embryos up to the blastocyst stage of life without risking or prejudicing the ones that are competent, in the whole process. Latest developed methods permit precise and regulated dynamic embryo culture with fluid flow.
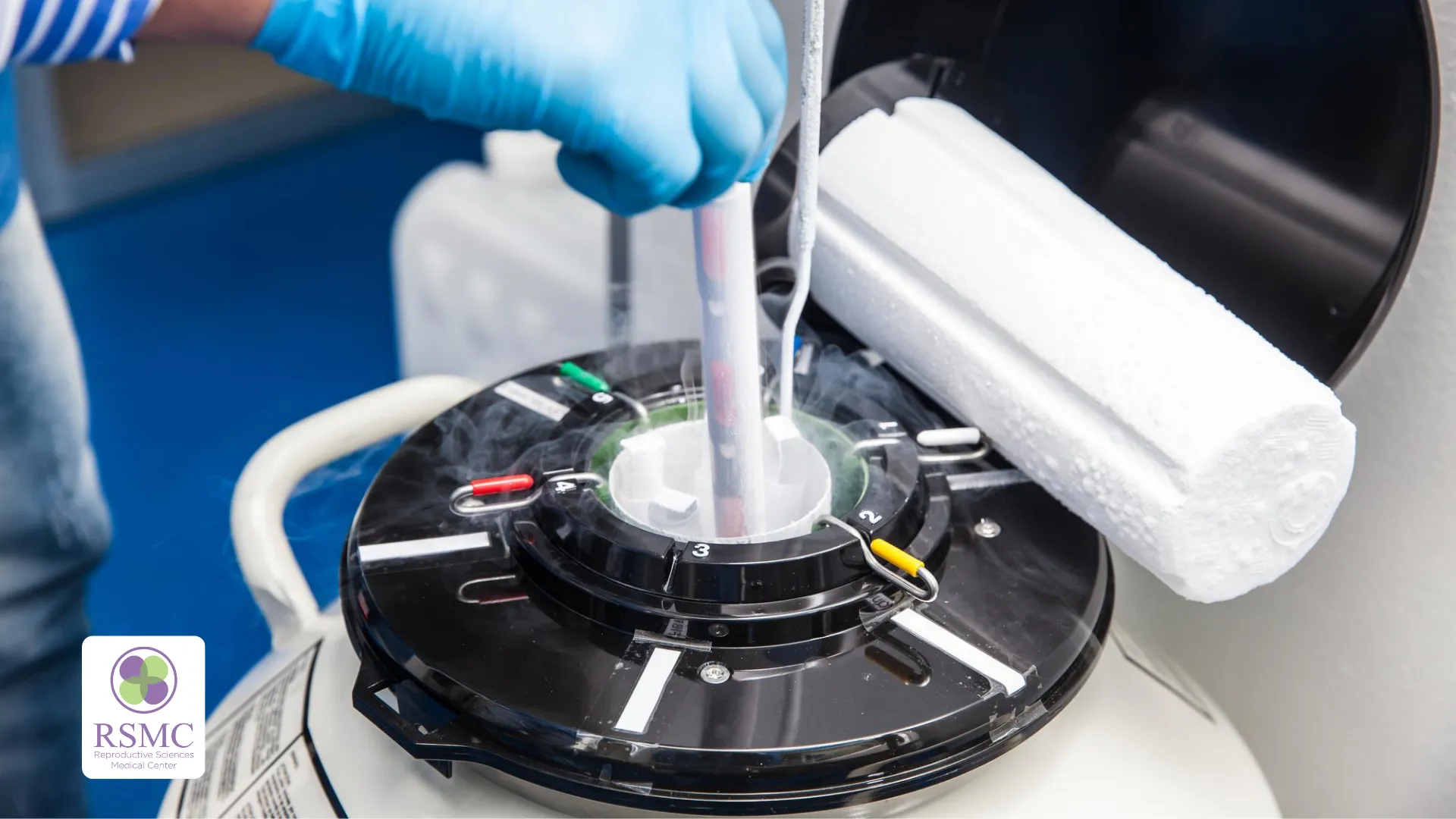
- Ultra-Rapid Embryo Freezing (Vitrification): Vitrification is a preserving technique developed to preserve eggs and embryos. This process leads to glass-like solidification of the eggs and embryos. Vitrification allows rapid freezing almost 600 times faster and much safer than conventional (slow) embryo freezing technique. Vitrification doesn’t allow ice to form inside, which protect the cells from damages. Using this process, we can store embryos safely and securely without worrying about them getting severely damaged by freeze-thaw processes. Vitrification technique ensures that the embryo’s potential to propagate as a baby remains the same as a freshly transferred embryo.
- Embryo Karyotyping Using CGH: the chromosomal integrity of the embryo has long been recognized as the “rate limiting factor” (the slowest step) in human reproduction. The embryos that have the incorrect number of chromosomes (more or less than the normal human genome of 46 chromosomes) in their cell have an increased risk of failed implantation or subsequent development. The aneuploid (embryo with an abnormal number of chromosomes) will either not attach to the uterine wall (unsuccessful implantation), attach for a short period of time before miscarrying, or result in the development and birth of a baby with a chromosomal disability such as Down Syndrome. Using preimplantation genetic diagnostic testing also referred as PGD, embryo chromosomal integrity is evaluated and only those embryos which are euploid (embryos that hold 46 chromosomes intact) are transferred. Some of PGD tests like fluorescence in-situ-hybridization (FISH), are incapable of identifying all 46 chromosomes and hence are unreliable to achieve perfection. New testing technique called comparative genomic hybridization (CGH), introduced approximately a decade ago, enabled identification of all 46 chromosomes in the human embryo’s cells. The advancement has improved selecting for the most “competent” embryos for transfer.
The journey from infertility to parenthood is not easy, but it surely is a joyful one with an irreplaceable goal. The happiness one feels holding their baby for the first time is priceless. When deciding which treatment option to go with, it is important to keep in mind the success rates as well as the health risks associated with each option. The single embryo transfer is a great option for many women and imposes less risks than multiple embryo transfers. If you are interested in consulting with a physician about the best option for you, please schedule a consultation with us.[/fusion_text][/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]