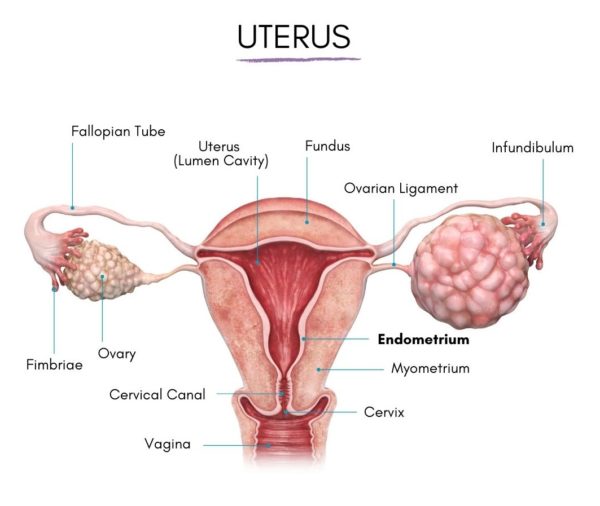
The endometrium refers to the inner lining of the womb/uterus. It is among the few tissues in a woman’s body that increase and decrease in size all through her reproductive years. Every month, the body prepares the womb lining to receive an embryo and the endometrial thickness changes during the process. Two female hormones, namely, progesterone and estrogen, cause the lining of the uterus to grow and shed through menstruation if a pregnancy doesn’t take place.
The normal thickness of the endometrium changes throughout a person’s life, from childhood, through to sexual maturity, her fertile years, and even after menopause.
What makes the womb lining thick or thin?
Although endometrial thickness normally changes during a female menstrual cycle, other factors can also bring about changes in the size of the uterus lining.
Pregnancy is one of the most common factors that can cause changes in endometrial thickness. Women who are less than five weeks pregnant or those carrying an ectopic pregnancy might show symptoms of a thickening womb lining.
Cancer of the ovaries or endometrial cancer is another condition that can cause the endometrium to thicken. As per the American Cancer Society (ACS), endometrial cancer is the most prevalent type of cancer affecting the female reproductive systems.
It is more common in white people than African Americans and rarely occurs in women below the age of 45. The average age that women are diagnosed with this condition is 60.
Other factors that can lead to an increase in endometrial thickness are:
- Diabetes
- Obesity
- Chronic high blood pressure
- Hormone replacement therapy
- Tamoxifen
- Scar tissue
- Endometrial hyperplasia
- Endometrial polyps
Thinning of Endometrium
Endometrial hyperplasia is a medical condition in which the lining of the womb becomes too thick. It is often due to insufficient progesterone and extremely high levels of estrogen or compounds similar to estrogen. Although this condition itself is not cancer, it can cause cancer to develop.
The womb lining (endometrium) can also be too thin. According to reproductive experts, endometrium that is not more than 7 mm is thin, and low endometrial thickness has been associated with age. However, reports show that 5% of women below 40 and 25% of those above 40 had a thin endometrium.
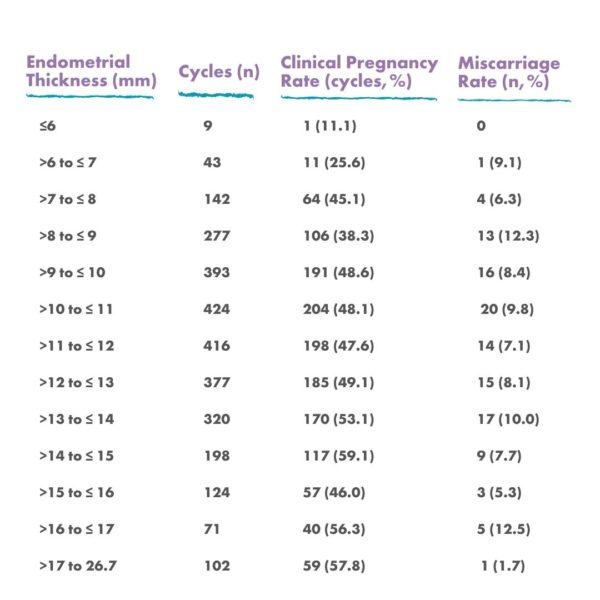
– Chart of Endometrial Thickness to Clinical Pregnancy Rate and Miscarriage Rate
Likely causes of a thin womb lining include medical treatment, inflammation, or the nature and structure of the endometrium itself.
Imaging tests of young women who are yet to begin menstruation show that they also have endometrium. It is just smaller than it will be later when they are grown.
According to an article by the Radiological Society of North America (RSNA), the endometrium is most thin during menstruation, usually between 2 to 4 mm thick.
The 1st half of the actively growing phase begins around day 6 to14 of a woman’s cycle or the period between the end of a menstrual cycle, when bleeding ceases, and prior to ovulation. At this phase, the womb lining starts to thicken and can measure around 5-7 mm.
The endometrium then becomes thicker (reaching up to 11 millimeters) as the cycle progresses and ovulation draws near,
Approximately 14 days to a woman’s cycle, hormones induce the release of an egg (ovulation). Endometrial thickness is at the highest during this phase and can be up to 16 mm.
How to measure
Ultrasound is the most commonly available option to measure the thickness of the endometrium. Healthcare providers use this method first, especially if an individual has reported abnormal vaginal bleeding.
When ultrasound is not suitable, (which is often due to the position of a person’s uterus or other health conditions) doctors resort to MRI.
Pregnancy
Endometrial thickness is very important during pregnancy.
Fertility experts have linked the best chances for a healthy, successful pregnancy to an endometrium that is not too thick nor too thin. This is because it enables the embryos to attach to the womb lining in order to obtain the nutrition it requires for survival. The lining of the uterus then becomes thicker and thicker as the pregnancy progresses.
Menopause
According to the RSNA, the endometrium usually measures around 5 mm or less in healthy postmenopausal women.
The womb lining, also known as endometrium, is where a growing embryo attaches to in the first few days of pregnancy. The thickness of the endometrium is, therefore, very important for women undergoing an IVF cycle. The fertility doctor will determine the thickness of the womb ling before the embryo is transferred to make sure it is thick enough to allow for implantation.
A nourishing, thick, receptive womb lining is the best environment for a developing embryo. And an ideal endometrium would be at least 7-8 mm thick and have a “trilaminar”(or 3-layered) appearance when checked through ultrasound.
An extremely thin womb lining can be a big issue during IVF, resulting in unsuccessful implantation or early pregnancy loss (miscarriage).
There are many reasons why a woman may have a thin womb lining, such as:
- Womb fibroids
- Estrogen deficiency
- Poor blood circulation to the womb
- Hydrosalpinx
- Adhesions or scar tissue in the womb due to infection or trauma
- Endometritis (inflammation of the endometrial cells)
Treatments options
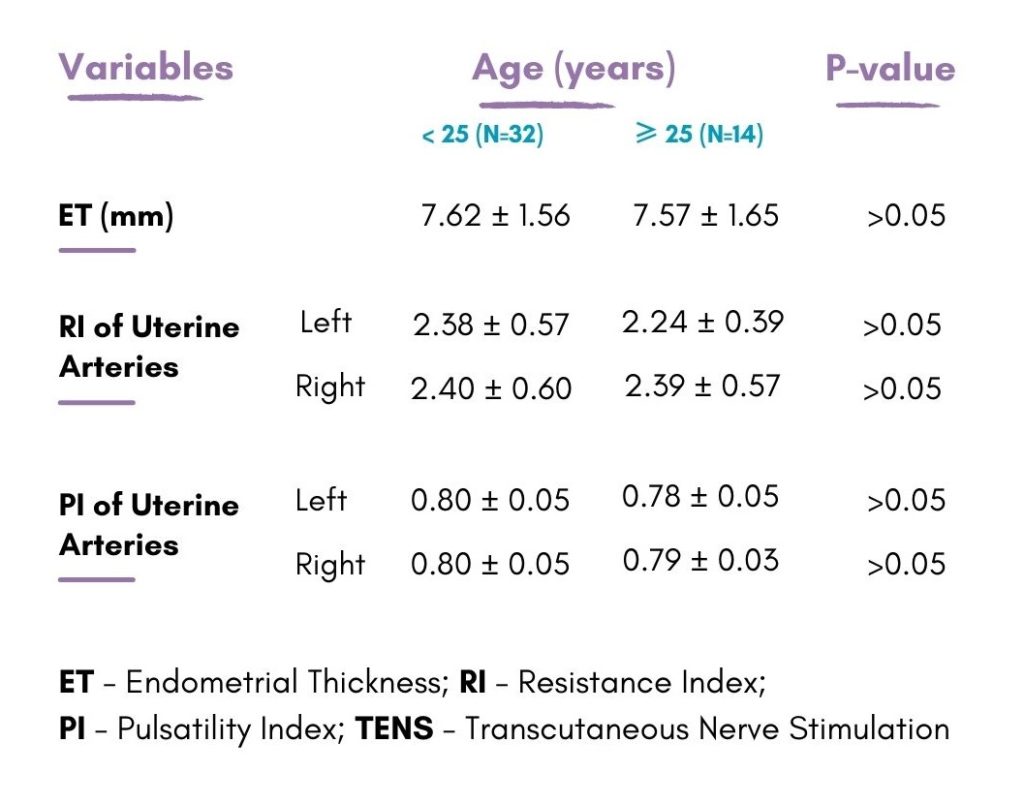
– Chart of measurement: The Effect of age on post-TENS of endometrial thickness, resistance, and pulsatility index for uterine arteries on both sides.
If your fertility doctor discovers that there’s an anatomical issue that can result in a too-thin womb lining, they may suggest that you first treat the problem before trying to conceive.
For instance, a slightly invasive surgery can be performed to repair a hydrosalpinx or remove fibroid tissues.
As for endometritis treatment, a short course of antibiotic medications can help treat the condition. For other issues, treatment often involved estrogen supplementation and taking steps to increase blood circulation to the pelvic area.
Although you can still conceive with a uterine lining that’s less than 7-8 mm thick, your physician may recommend that you try to thicken your womb lining before undergoing the embryo transfer procedure. Below are some ways you can promote the growth of your endometrium.
Treatments for extremely thick endometrium include progestin (an artificial hormone that prevents ovulation) and hysterectomy (surgical removal of the womb).
According to studies, it is also harder for a pregnancy to progress when a woman has a thin uterine lining. Treatments for extremely thin endometrium include:
1. Take estrogen supplements
The doctor may recommend that you take estrogen supplements, whether in the form of patches, oral pills, or suppositories. This is referred to as “exogenous” estrogen. In certain cases, your doctor may suggest that you undergo an rFSH treatment like Gonad-F to encourage your body to produce more natural estrogen. This is called “endogenous” estrogen.
2. Improve your blood circulation
The womb needs a good supply of blood to develop a thick endometrial lining. Therefore, improving blood circulation throughout your body is one of the best ways to promote the growth of your endometrium.
-
Exercises
Also, engage in moderate exercise regularly as it helps with blood flow. A lot of us are living a sedentary lifestyle nowadays, working desk jobs that keep us on our seats for hours.
During this period, our blood circulation slows down, and our reproductive organs are compressed. Hence, it is important to be moving your body if you are trying to increase the thickness of your womb lining. When you increase your heart rate, you increase the flow of fresh, oxygenated blood throughout your body.
Remember not to exercise too much, though: high-impact or high-intensity exercise is not needed or recommended for patients undergoing an IVF cycle. However, bike rides, short walks, yoga classes, or 30 minutes on an elliptical machine at a slow pace are excellent ways to improve your blood flow. You can carry out this kind of exercise daily without stressing your body too much.
-
Reduce substance abuse
Reduce or stay away from substances that can affect blood circulation. For example, nicotine and caffeine are bad for your blood flow: stop smoking and limit your coffee intake to one cup per day. Some medications for cold and seasonal allergies that help prevent nasal inflammation may also constrict the veins. So, consult with your physician regarding which medications you should not take at this time.
-
Consider acupuncture.
A lot of women find acupuncture helpful during this treatment stage. While research on the impacts of acupuncture on fertility is still ongoing, some studies indicate that it can assist with blood circulation.
-
Viagra suppositories as per recommendation
Ask your physician about Viagra suppositories. Although Viagra is often used to promote blood circulation to the penis in men with erectile dysfunction (ED), it can also be used to improve the flow of blood to the female pelvic area by using vaginal suppositories.
-
Body weight and BMI
Check your body weight. If you have a low BMI, you may want to add a little flesh with the assistance of a nutritionist. Additional weight can improve blood circulation to the pelvic region. Plus, adipose cells produce extra estrogen. You should aim for a BMI (basal metabolic index) in the range of 18.5 to 24.9.
2. Research nutritional supplements
Although there is no proof that the use of herbs, vitamins, and supplements helps increase endometrial thickness, some studies have suggested that they can help. For instance, supplemental tocopherol (vitamin E) and L-arginine can be associated with improvements in the womb lining. Also, vitamin D deficiency can reduce the chances of successful implantation. However, you need to do your homework properly and consult with your physician before you start taking any new supplement.
3. Consider Frozen Embryo Transfer (FET)
The ovarian stimulation cycle and egg retrieval procedure can be hard on your body and fertility hormones. Some reproductive experts think that women who have issues with their endometrial thickness may have better implantation chances if they freeze their embryos after IVF and defer transfer until one or two months later when their body has fully recovered from the fertility drugs. The success rates of a FET cycle compare favorably to those of a fresh embryo transfer cycle.
In certain cases, resting gives the reproductive system an opportunity to “reset” and allows the body to commit its energy to develop a thick uterine lining.
4. Getting the “ideal” endometrial thickness
Although there have been cases of women with uterine lining as thin as 4 mm who got pregnant and delivered a healthy baby, it will be hard for you to conceive if your womb lining is not thick enough. However, if you are worried about an extremely thin endometrium and want to know how we can help, contact RSMC today to schedule a consultation with our experts.