What is an ectopic pregnancy?
An ectopic pregnancy is a pregnancy complication in which the embryo attaches outside the cavity of the womb, usually in the fallopian tubes. Ectopic pregnancy is also known as
- EP
- Tubal pregnancy
- Fallopian tube pregnancy
- Eccyesis
- Extrauterine pregnancy
- EUP
- Abdominal pregnancy
- Cervical pregnancy
The first known mention of tubal pregnancy is traced back to the 11th century by Al-Zahrawi – a famed Arab physician/surgeon. The term “ectopic” itself means “out of place”.
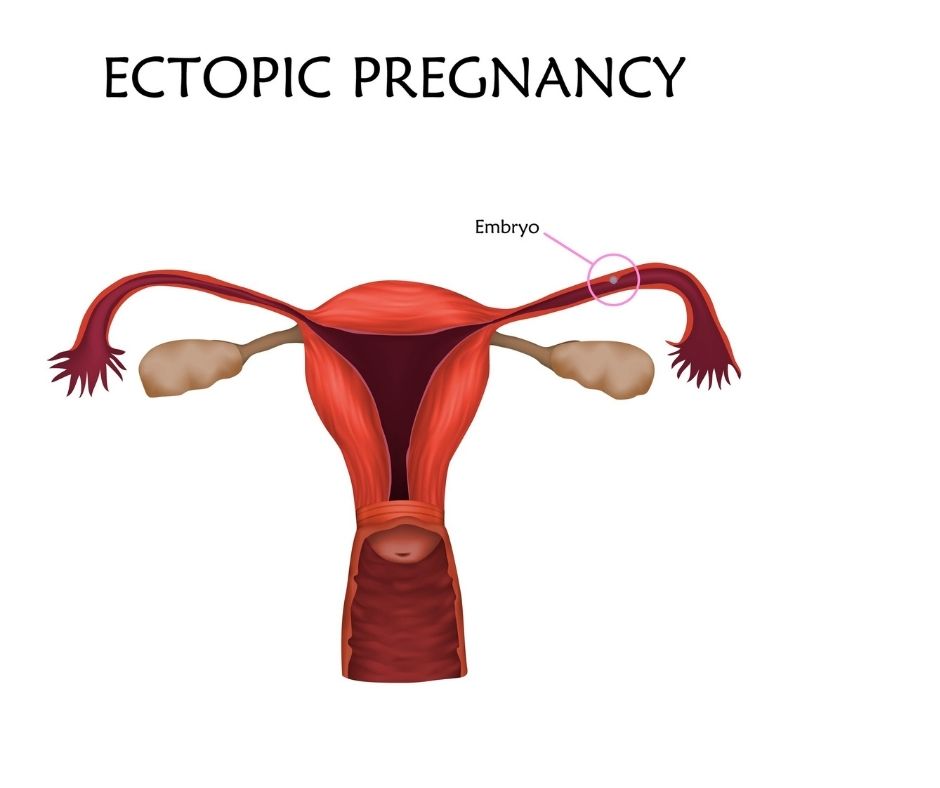
How it happens
Normally, the fertilized egg attaches to and grows in the uterus. But in most ectopic pregnancies, the egg lodges in the fallopian tubes instead of continuing on its journey to the womb. And this is why they are often referred to as tubal pregnancies. Other places where the fertilized egg can also implant include the ovary, cervix, or abdomen. Hence, they may also be called abdominal or cervical pregnancies.
Unlike the uterus, these areas do not have much space or the nurturing tissue to grow a pregnancy. As the fetus develops, it will ultimately rupture the organ containing it, causing heavy bleeding and putting the mother’s life in danger. A typical ectopic pregnancy does not result in a live birth.
What are the symptoms and signs of ectopic pregnancy?
The three common symptoms of ectopic pregnancy are vaginal bleeding, absence of menstruation (amenorrhea), and abdominal pain. However, just 50% of women experience all of these symptoms.
- Sharp pain in the pelvis, abdomen, neck, or shoulder
- Light to heavy vaginal bleeding or spotting
- Pain on one side of the belly
- Fainting or dizziness
- Pressure in rectum
If you are pregnant and are experiencing any of these symptoms, contact your physician or seek treatment as soon as possible.
What causes an ectopic pregnancy?
An ectopic pregnancy occurs when a fertilized egg settles in the uterine tube or other locations outside the womb, where it should implant. The egg may get stuck when this tube is distorted, damaged, or scarred.
Although the cause of ectopic pregnancy is sometimes unclear, it is often linked to these conditions:
- Genetic disorders
- Hormonal factors
- Birth defects
- Scarring and inflammation of the fallopian tubes due to an infection, surgery, or an underlying health condition that alters
- The shape of the fallopian tubes and other reproductive structures.
What are the possible risk factors for ectopic pregnancy?
Any sexually active woman can have an ectopic pregnancy. However, the risk increases with any of the following:
- Reproductive age of 35 yrs or above
- Smoking
- History of endometriosis
- History of pelvic inflammatory disease
- Conceiving despite intrauterine device (IVD) or tubal ligation
- Conceiving through fertility medications or procedures
- History of sexually transmitted infections like gonorrhea or chlamydia
- History of abdominal surgery, pelvic surgery, or several abortions
- Having structural issues in the Fallopian tube makes it difficult for the egg to pass through it.
- History of ectopic pregnancy
How these factors raise the risk of having an ectopic pregnancy
1. Age
Any woman – regardless of age – who is ovulating and has sex with a man can develop an ectopic pregnancy. However, women between the ages of 35 and 44 are most likely to have the condition.
2. History
A previous history of ectopic pregnancy is the biggest risk factor for having another ectopic pregnancy.
3. Abnormalities in the fallopian tubes
Any disruption of the normal structure of the uterine tubes can result in a tubal pregnancy or pregnancy in other places outside the womb.
4. Past gynecological surgeries
Past surgery on the fallopian tubes can cause scarring and disruption of the normal architecture of these tubes, raising the chances of an ectopic pregnancy.
5. Infections
Another thing that can increase your risk of ectopic pregnancy is pelvis infections. These infections may be caused by sexually transmitted bacteria like N. gonorrhea or chlamydia or by other bacteria transmitted through other means. They can cause an ectopic pregnancy by blocking or damaging the fallopian tubes.
The inner lining of the uterine tubes has small hair-like projections known as cilia. These cilia help the egg travel from the ovary through the fallopian tube and into the womb. The damage of these cilia by infection can disrupt egg transport in the uterine tube. Hence, the fertilized egg may become stuck in the tube (unable to reach the womb), leading to an ectopic pregnancy. Similarly, infections can cause scarring and partial blockage of the fallopian tubes, preventing the egg from getting into the uterus.
6. Multiple sex partners
The more sex partners a woman has the higher her chances of pelvic infections. Hence, having more than one sex partner may increase the likelihood of an ectopic pregnancy.
7. Gynecological conditions
Conditions like endometriosis, fibroid tumors, or pelvic adhesions can cause the fallopian tubes to become narrow and hinder egg transport, hence raising the risk of an ectopic pregnancy.
8. Use of intrauterine device (IUD)
Nearly 50% of pregnancies in women using IUDs will develop outside the womb. However, only a few women get pregnant when using intrauterine devices. So, the total number of ectopic pregnancies linked to IUDs is pretty low.
9. Cigarette smoking
Smoking cigarettes around the time of conception increases the risk of ectopic pregnancy. However, this risk was found to be dose-dependent. This implies that the risk increases with the number of cigarettes smoked and depends on the woman’s personal habits.
10. Infertility
A history of infertility for years has also been linked with a higher risk of ectopic pregnancy.
11. Other possible causes
Birth defects, infection, or fallopian tube tumors can raise a woman’s risk of having a tubal pregnancy.
What is the percentage of women who have an ectopic pregnancy?
Around 1 to 2 % of all pregnancies are ectopic.
What tests, exams, or medical procedures are used to diagnose ectopic pregnancy?
If you think that you might have an ectopic pregnancy, consult your doctor as soon as possible. Although ectopic pregnancies cannot be detected by a physical examination, your physician may still conduct one to eliminate other possible factors.
Normal examination
The first step in ectopic pregnancy diagnosis is an interview and physical examination by a physician.
Pregnancy tests
The second step is to get a quantitative (determines hormone levels) or qualitative (positive or negative for pregnancy) pregnancy test. Usually, the physician may notice a tender mass during the pelvic exam. If the doctor suspects an ectopic pregnancy, blood pregnancy tests and pelvic ultrasound may be performed.
Transvaginal ultrasound test
The next step to diagnose an ectopic pregnancy is a transvaginal ultrasound (also called endovaginal ultrasound). Transvaginal ultrasound is the ideal test to check female reproductive organs for an ectopic pregnancy. In this test, the doctor inserts a small wand-like instrument into the vagina and pelvic images are seen on a monitor to check if the uterus contains a gestational sac.
But while this ultrasound can show the gestational sac in a normal pregnancy or an ectopic pregnancy, the findings are usually inconclusive. Instead of a gestational sac housing an embryo, the ultrasound may show a small mass in the fallopian tubes or other places, suggesting an ectopic pregnancy. It can also let you know if there’s no pregnancy at all.
Laparoscopy
Laparoscopy may also be required to establish a diagnosis of ectopic pregnancy. During a laparoscopic examination, optical instruments are inserted through tiny incisions in the abdomen to see the structures in the pelvis and abdomen, showing the location of the ectopic pregnancy.
Hormone test
Your physician may also perform a blood test to examine your levels of pregnancy hormones, such as progesterone and human chorionic gonadotropin (HCG). If the levels of these hormones begin to decrease or remain unchanged for a couple of days and a gestational sac is not seen during an ultrasound, then the pregnancy may be ectopic.
Note: If you are experiencing severe symptoms, like bleeding or sharp pain, there may not be adequate time to undergo all these steps. In extreme cases, the fallopian tube may burst, causing serious internal bleeding. Your physician will have to carry out emergency surgery to offer immediate treatment.
Ectopic pregnancy treatment
Ectopic pregnancies are dangerous for the mother. Plus, the embryo will be unable to develop to full term. Therefore, it is important to remove the embryo ASAP to ensure the mother’s health and future fertility. Fortunately, there are various treatment options you can consider, depending on the site of the ectopic pregnancy and its development.
Medication
If your physician thinks that immediate complications are unlikely, he or she may recommend medications that could prevent the ectopic mass from rupturing. One medication often recommended for this is methotrexate.
Methotrexate hinders the growth of quickly dividing cells like the cells of the ectopic mass and is usually taken in the form of an injection. Note that it’s important to undergo regular blood tests to be sure that the medication is working. If it is effective, you will experience symptoms like those of a miscarriage, such as:
- Bleeding
- Cramping
- The passing of tissue
There is usually no need for further surgery after this happens. Methotrexate does not pose risks of fallopian tube damage, unlike surgery. However, you will not be able to conceive for many months after using this medication.
Surgery
A lot of surgeons recommend a laparotomy – a medical procedure to remove the embryo and repair internal damage. During this surgery, the doctor will insert a tiny camera through a small incision on the abdomen to be able to see their work.
If the surgery does not succeed, the doctor may do another laparotomy, this time using a larger abdominal incision. He or she may have to remove the fallopian tube if it is severely damaged.
Home care
Your physician will provide you with a set of instructions regarding the care of your abdominal incisions post-surgery. You have to make sure your incisions are kept clean and dry as they heal. So, check them every day for signs of infection, including:
- Redness
- Swelling
- Hot to the touch
- Foul-smelling drainage from the incision site
- Continuous bleeding
- Heavy bleeding
You may experience blood clots and vaginal bleeding post-surgery. This can happen up to 6 weeks following the procedure. Here are some self-care measures you may take:
- Avoid lifting anything heavier than 10 pounds
- Take a lot of fluids to prevent constipation
- Have pelvic rest. This means staying away from sex, douching, and using tampons.
- Rest as much as you can the first week after surgery, and then raise your activity level in the following weeks.
- Always inform your physician if your pain becomes more intense or you feel like something is not okay.
Prevention
Unfortunately, there is no way you can predict or prevent ectopic pregnancies. You can only minimize the risk by maintaining good reproductive health. Ensure that your partner uses a condom during intercourse and reduce the number of people you have sex with. This lowers your risk of contracting sexually transmitted diseases, which may cause pelvic inflammatory disease, a condition that can damage the fallopian tubes.
Visit your doctor regularly and undergo all the necessary STD screenings and gynecological examinations. It will also be good to take steps to enhance your health, like quitting smoking.
What’s the outlook after an ectopic pregnancy?
This depends on whether the pregnancy resulted in any physical damage to your reproductive organs. A lot of women who have an ectopic pregnancy later have healthy pregnancies. The egg can become fertilized as long as one of the fallopian tubes remains intact. But if you have an underlying fertility issue, that can impact your fertility later on and raise your risk of having an ectopic pregnancy in the future. This is usually the case if the underlying fertility issue has previously caused an ectopic pregnancy.
Surgery can cause scarring of the fallopian tubes, increasing the likelihood of future ectopic pregnancies. If it is necessary to remove one or both fallopian tubes, consult your physician about possible fertility treatments, i.e., in vitro fertilization (IVF), which involves the transfer of a fertilized egg into the womb.
Bottom line
Losing a pregnancy can be a devastating experience, no matter how early it occurs. So, ask your physician if there are any local support groups that can offer emotional support after the pregnancy loss. Make sure to take good care of yourself after the pregnancy loss by resting, consuming healthy foods, and exercising when you can. Allow yourself enough time to grieve.
Bear in mind that a lot of women have healthy pregnancies and babies after an ectopic pregnancy. If you are not sure, what would be the right options for you, schedule a consult with RSMC fertility specialists about ways to make sure you have healthy pregnancies in the future.